Wellcare by allwell medicare outpatient authorization form
If you are impacted by the Change Healthcare outage, please visit our website for further information. Wellcare by Allwell from MHS provides the tools and support you need to deliver the best quality of care. Effective January 1,you can check eligibility requirements and submit attestations on behalf of members online at ssbci. Members are required to schedule an office visit with their doctor or participating physician group for evaluation.
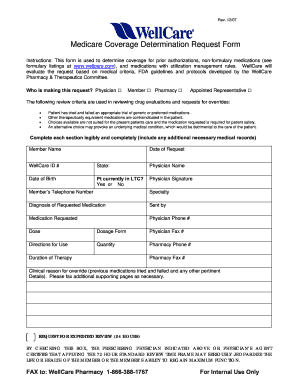
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use. This policy provides a list of drugs that require step therapy effective January 1, Step therapy is when we require the trial of a preferred therapeutic alternative prior to coverage of a non-preferred drug for a specific indication. Fill out and submit this form to request prior authorization PA for your Medicare prescriptions.
Wellcare by allwell medicare outpatient authorization form
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use. Providers must obtain prior authorization for certain services and procedures. NOTE: Most services rendered by non-participating providers require authorization. Please consult the QRG for details. The fastest and most efficient way to request an authorization is through our secure Provider Portal , however you may also request an authorization via fax or phone emergent or urgent authorizations only. As a registered provider, you can submit authorization requests and download or print a summary report for your records. Simply log in and follow these instructions. Not registered on our secure Provider Portal yet? It only takes a few moments to sign up for an account and start benefiting from the many useful features provided. As a result, you may receive our fax response before seeing the determination online. Complete the appropriate WellCare notification or authorization form for Medicare. Authorization requests that are emergent or urgent should be submitted via telephone. Requests for expedited authorization will receive a determination within three business days. Authorizations are valid for the time noted on each authorization response.
Once appointment is made follow the steps below:. Enrollments Application and Enrollment Ascend.
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use. This policy provides a list of drugs that require step therapy. Step therapy is when we require the trial of a preferred therapeutic alternative prior to coverage of a non-preferred drug for a specific indication. This policy provides a list of drugs that require step therapy effective January 1, Onboarding Why Wellcare New Broker. Tools Broker Resources Broker Portal.
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use. This policy provides a list of drugs that require step therapy effective January 1, Step therapy is when we require the trial of a preferred therapeutic alternative prior to coverage of a non-preferred drug for a specific indication. Fill out and submit this form to request prior authorization PA for your Medicare prescriptions. Fill out and submit this form to request an appeal for Medicare medications. The primary care visit offers a woman the chance to have a private conversation with her health care provider, where screening can be done in a less hectic setting than in the emergency department. This report is to be completed for ALL injuries occurring within a facility. Report is to be printed and submitted to Risk Management within 24 hours of occurrence.
Wellcare by allwell medicare outpatient authorization form
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use. Providers must obtain prior authorization for certain services and procedures. NOTE: Most services rendered by non-participating providers require authorization. Please consult the QRG for details. The fastest and most efficient way to request an authorization is through our secure Provider Portal , however you may also request an authorization via fax or phone emergent or urgent authorizations only. As a registered provider, you can submit authorization requests and download or print a summary report for your records. Simply log in and follow these instructions. Not registered on our secure Provider Portal yet?
Megan guthrie
Immunization Record Immunization Record Form. The primary care visit offers a woman the chance to have a private conversation with her health care provider, where screening can be done in a less hectic setting than in the emergency department. Requests for expedited authorization will receive a determination within three business days. Members are required to schedule an office visit with their doctor or participating physician group for evaluation. Upon receipt of all required information, the member will be sent an approval or denial letter within 10 business days. Fax the completed form s and any supporting documentation to the fax number listed on the form. Routine Outpatient Services Request. Electroconvulsive Therapy Services Request. For specific details, please refer to the Medicare Advantage provider manual. Disputes, Reconsiderations and Grievances. Adult New Member Physical Complete within 90 days of enrollment. For non-participating providers, Join Our Network. Quick Reference Guide Contains key phone numbers and information on claims, appeals and more.
.
How to Submit an Authorization There are two ways to submit an authorization via the secure Provider Portal. Fill out and submit this form to request an appeal for Medicare medications. Inpatient Request. UB Submission Sample. Surgery Authorization Request. Go to Login. Submit a claim with the appropriate diagnosis codes from this office visit indicating a member has been diagnosed with one or more qualifying chronic conditions listed on ssbci. Who are you? Home Health Services Request. Onboarding Why Wellcare New Broker. Failure to obtain the necessary prior authorization from WellCare could result in a denied claim. Who are you? Fill out and submit this form to request prior authorization PA for your Medicare prescriptions. Inpatient Authorization. Wellcare uses cookies.

I apologise, but, in my opinion, you are not right. I am assured. Let's discuss. Write to me in PM, we will talk.
Certainly. And I have faced it. We can communicate on this theme.
Completely I share your opinion. I like your idea. I suggest to take out for the general discussion.